In today’s rapidly evolving healthcare landscape, claims process automation is revolutionizing how healthcare providers and insurance companies manage their operations. This automation is not just about speeding up processes but ensuring accuracy, minimizing costs, and enhancing the overall customer experience. One standout tool in this arena is Kudra, an AI-powered platform designed to streamline data extraction from healthcare insurance claims and other documents.
By embracing claims process automation through Kudra, organizations can dramatically reduce the time spent on manual data entry and processing, paving the way for greater operational efficiency. This in-depth guide will explore not only the steps involved in using Kudra for automating the claims process but also the broader impacts of automation on the healthcare industry.
The Importance of Claims Process Automation in Healthcare
Claims process automation is critical for healthcare providers and insurance companies, where the volume of claims can reach staggering levels. Traditionally, claims management has been a manual, error-prone process that involves entering data from paper forms, cross-referencing with policy information, validating claims, and eventually approving or denying them.
The manual approach has several inherent issues:
- Increased Errors: Manual data entry increases the likelihood of errors, leading to rework and delays.
- High Costs: Managing claims manually requires significant labor, adding to operational costs.
- Slow Turnaround: Claims processing can take days or weeks, frustrating patients and insurance companies.
Claims process automation, especially when using an AI tool like Kudra, addresses these issues by streamlining the data extraction process, improving accuracy, and drastically reducing processing time.
The Role of AI in Claims Process Automation
Artificial Intelligence (AI) and Machine Learning (ML) are transforming how businesses approach automation. In the context of claims process automation, AI can automatically read, understand, and process data from healthcare claim forms.
Here’s how AI plays a pivotal role:
• Data Extraction: AI-powered systems like Kudra can scan and extract key information from documents, whether they’re PDFs, scanned images, or text files. This eliminates the need for manual data entry.
• Pattern Recognition: Machine learning models can identify patterns in data, allowing Kudra to continually improve its accuracy over time.
• Error Reduction: AI tools can cross-check information, validate entries, and flag inconsistencies, drastically reducing human errors.
As AI evolves, so does its potential to handle more complex claims scenarios, making it an indispensable part of claims process automation.
How Kudra Enables Seamless Claims Process Automation
Kudra stands out in the world of claims process automation due to its versatility, user-friendly design, and powerful AI-driven capabilities. At the core of Kudra’s offering is its ability to extract critical information from claim forms with minimal human intervention. Here’s a more detailed look at how Kudra enables automation:
Step 1: Setting Up the Kudra Workflow
The foundation of Kudra’s power lies in its workflow customization. From the Workflows page, users can select pre-built workflows designed specifically for healthcare claims or create custom workflows based on their needs.
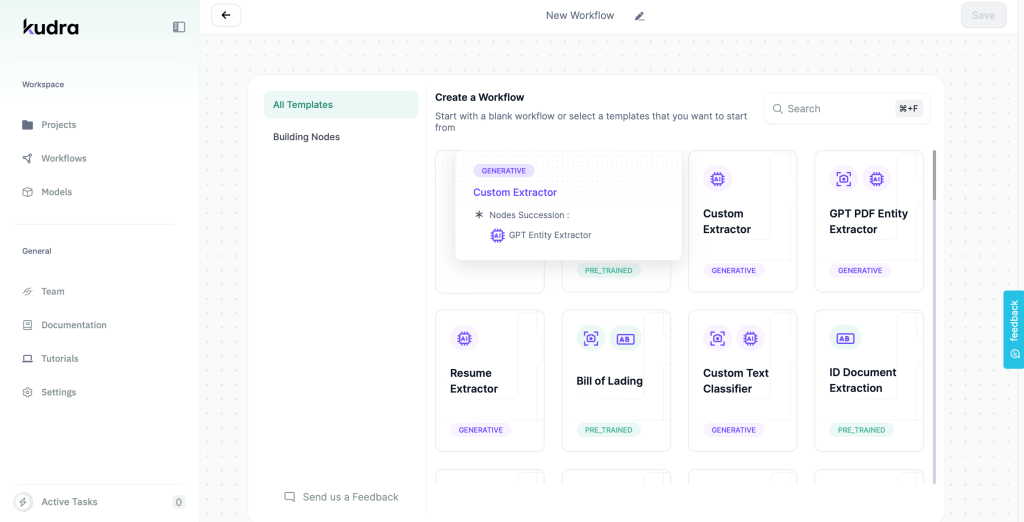
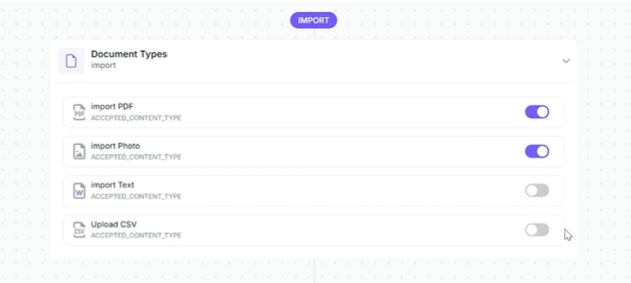
• Document Import Options: Kudra supports a wide range of document types, including PDFs, text files, CSVs, and even images. Users can enable or disable these import types based on their specific use case, ensuring flexibility.
• Drag-and-Drop Interface: The platform’s simple drag-and-drop interface allows users to build custom workflows with ease, configuring every step of the document processing journey.
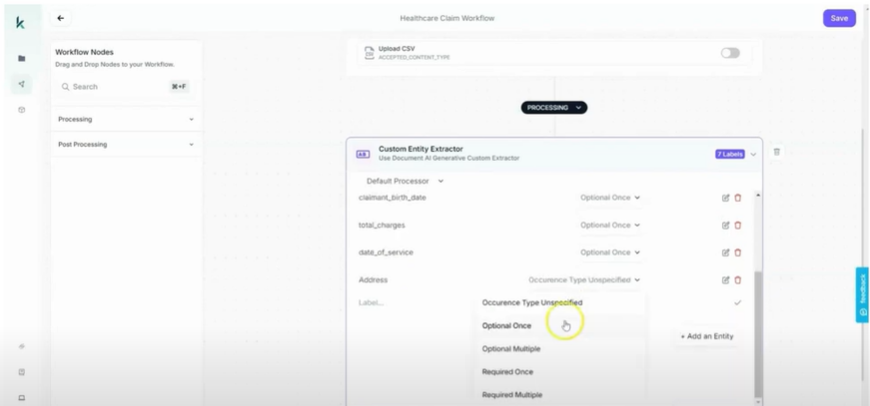
Step 2: Custom Entity Extraction
This is where Kudra’s AI shines. The Custom Entity Extractor allows users to specify exactly what data points need to be extracted from the claim forms. These can include:
- Patient Information: Claimant’s name, birthdate, and address.
- Insurance Details: Policy number and provider information.
- Medical Information: Date of service, description of service, diagnosis codes, and total charges.
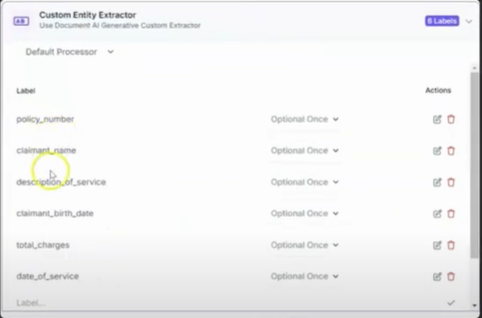
Once these entities are defined, Kudra’s AI learns how to identify them in future claims, making the system smarter with each document processed.
Step 3: Entity Occurrence Customization
In claims processing, different data points may appear once, multiple times, or optionally in a document. Kudra’s customization options allow users to set these occurrences to “Optional Once,” “Required Once,” or “Multiple” depending on how often the information appears. This level of precision is critical for ensuring that the AI accurately captures all relevant information without flagging false positives.
Advanced Data Processing Features in Kudra
While extracting data is central to claims process automation, Kudra offers additional features that enhance its capabilities:
Error Detection and Validation
One of the biggest challenges in healthcare claims processing is the potential for errors. These can range from missing information to incorrect codes or charges. Kudra’s AI uses machine learning to validate the extracted data, checking for discrepancies such as:
- Incorrect policy numbers
- Mismatched dates of service
- Missing medical codes
In cases where the AI detects inconsistencies, it can flag the document for human review, allowing for a semi-automated approach that minimizes errors while ensuring compliance with healthcare regulations.
Scalability and Bulk Processing
For large healthcare providers or insurance companies, processing hundreds or thousands of claims daily is common. Kudra’s platform is built to scale, allowing users to upload and process massive volumes of documents simultaneously. Bulk processing capabilities mean that entire batches of claim forms can be automated in minutes, significantly reducing the time to process each claim.
Automated Workflow Triggers
Kudra also supports automated workflow triggers, allowing users to set conditions that automatically initiate processes based on certain criteria. For example:
- When a new claim is uploaded, Kudra automatically extracts the necessary information.
- If a claim is missing key data points (e.g., claimant name), the system can trigger an alert for manual review.
These triggers help to create a fully automated, hands-off approach to claims processing, freeing up human resources for more complex tasks.
Integrating Kudra into Existing Systems
For maximum efficiency, claims process automation solutions need to integrate seamlessly with other software systems, such as Electronic Health Records (EHR), claims management platforms, and billing software. Kudra offers multiple integration options:
• API Access: Kudra provides robust APIs that allow it to integrate with other systems, enabling the automatic transfer of data between platforms.
• Data Export Options: After processing claims, Kudra allows for easy data export in various formats (CSV, XML, etc.), which can be uploaded directly into an organization’s claim management system.
• Real-Time Syncing: Kudra supports real-time syncing, ensuring that data processed through Kudra is instantly reflected in other systems, reducing lag time between claim submission and resolution.
With these integrations, Kudra becomes part of a larger ecosystem of tools, streamlining not just data extraction but the entire claims process automation pipeline.

Security and Compliance in Claims Process Automation
Security and compliance are critical in healthcare due to strict regulations like HIPAA (Health Insurance Portability and Accountability Act). Kudra takes these concerns seriously by implementing:
Data Encryption
All data processed through Kudra is encrypted, both in transit and at rest. This ensures that sensitive patient information remains protected, meeting the strict requirements of HIPAA and other data protection regulations.
Access Controls and User Permissions
Kudra allows administrators to set strict access controls, ensuring that only authorized personnel can view or edit sensitive data. Role-based access helps protect against unauthorized data breaches while maintaining accountability.
Audit Trails
For healthcare providers and insurance companies, maintaining detailed records of how claims are processed is crucial for compliance. Kudra automatically generates audit trails, tracking every action taken on a document, from data extraction to validation and export. These logs can be essential for both internal audits and regulatory inspections.
Benefits of Automating Healthcare Claims with Kudra
Increased Efficiency and Productivity
With Kudra’s claims process automation, healthcare providers and insurers can significantly reduce the time it takes to process claims. AI-driven data extraction works faster than humans, and with bulk processing capabilities, hundreds of claims can be managed simultaneously.
Cost Savings
By automating labor-intensive tasks like data entry and validation, organizations can drastically reduce operational costs. Employees can focus on higher-value tasks like customer service and issue resolution rather than manual data processing.
Improved Accuracy
Kudra’s AI-powered extraction reduces human error, ensuring that the information is captured accurately and consistently. This leads to fewer claim rejections due to mistakes and faster claim approval rates.
Compliance and Risk Reduction
By automatically validating data and ensuring compliance with healthcare regulations, Kudra helps organizations mitigate the risk of non-compliance penalties and ensures that claims meet industry standards.
The Future of Claims Process Automation
In the modern healthcare landscape, the ability to efficiently process insurance claims can make a significant difference in operational costs, patient satisfaction, and regulatory compliance.
By automating tasks that were once manual, time-consuming, and error-prone, Kudra enables organizations to process claims faster, with greater accuracy, and at a lower cost. Its flexibility in handling various document formats, custom data extraction workflows, and scalable processing capabilities make it an ideal solution for healthcare providers of all sizes.
By incorporating Kudra into your claims processing workflow, you’re not just improving efficiency; you’re setting the stage for a future where healthcare administration is faster, smarter, and more responsive to the needs of both patients and providers. Claims process automation is here to stay, and Kudra is leading the charge.